Introduction
Major thalassemia (TM) and sickle cell disease (SCD), two common genetic hemoglobinopathies, were often fatal 50 years ago. Novel therapeutic and diagnostic methods are increasing lifespan and quality of life. Recent advances in iron chelation for transfusion-dependent hemoglobinopathies have significant improved patient prognosis.
Young adult TM and SCD patients often ask about the possibility of conception and pregnancy.
The increase in the worldwide movement of carriers and subjects has lead to new cultural, ethical and psychosocial aspects that must be taken into consideration.
The present study investigated the fertility rate, maternity/paternity status, need for assisted reproductive techniques (ART), abortion rate, pregnancy/newborn complications in patients with hemoglobinopathies.
Methods
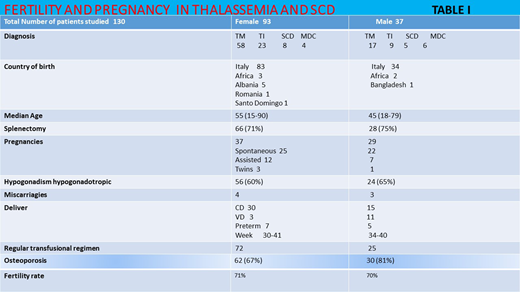
We followed 130 female (FPs) and male (MPs) patients (F:M=93:37); 75 with TM, 32 with thalassemia intermedia (TI), 13 with SCD and 10 with microdrepanocytosis (MDC).
Median age is 55 yo (15-90) for TM+TI and 45 yo (18-79) for SCD+MDC. Pregnancy was reported in 37/52 FP of childbearing age (15-49 yo), and conception in 15 MP with fertility rates of 71% and 70%, respectively.
Results
We reviewed 66 conceptions from 1999 to 2020.
Mother age at pregnancy was between 32-39 yo. Forty-seven pregnancies were spontaneous and 19 medically assisted. There were 3 ovodonations and 2 ICSI; 64% of pregnancies were planned.
Pregnancy outcomes of 22 TM, 16 TI, 8 SCD and 3 MDC patients are described.
There were 7 miscarriages in the first 12 weeks: 3 in TI, 1 in SCD FP; 1 in TM and 2 in SCD MP. Abortion rate was 9%, comparable to the general population.
Intrauterine death at 24w occurred in a SCD FP for placental thrombosis and eclampsia.
Sixty live healthy newborns were delivered;4 twin pregnancies occurred (1 TM MP, 3 TM FP).
Only 1 malformation was observed, in an infant born after ovodonation in a TM FP who had minor gastroenteric and urinary malformations that were surgically corrected.
Obstetric complications were eclampsia, disseminated intravascular coagulation, cardiac failure, and acute chest syndrome in SCD patients. One ovarian hyperstimulation syndrome in the 1st month of pregnancy with ascites and admission to the ER was reported.
There were 30 (94%) caesarians (CD) and 3 vaginal deliveries (VG) in FP, with 7 preterm babies (22%). In partners of MPs there were 15 CD (56%), and 11 VG with 5 preterm babies (Table I).
Births from MPs occurred between 34-40w with a median birth weight of 3 kg (2.17-4) and 30-41w in FPs with a median birth weight of 2,5 kg (1,1-3,4) .
FPs were able to breast fed in 56% of cases for a medium time of 66 days (20-120), while female partners of MPs breastfed for 193 days (20-540).
Newborn events includes 14 jaundices; 9 babies were placed in intensive care and required incubator use due to cerebral hemorrhage or infections requiring antibiotic therapy.
Discussion
Spontaneous pregnancies occur in well chelated and transfused patients but a relevant part of those patients are infertile due to hypogonadism due to transfusional hemosiderosis and may need ART.
These patients present a base-line pro-coagulant state which can worsen during pregnancy, needing antithrombotic prophylaxis and require regular consultations, since pregnancies are considered high risk for both mother and baby. As osteopenia-osteoporosis are the common endocrine complications in hemoglobinopathies (67% of FPs), both cesarean delivery and breast feeding are strongly suggested. Even though chelating therapy during lactation does not alter iron excretion, our patients didn't receive chelating therapy when breastfeeding.
Multidisciplinary programs including transfusions, cardiac and clinical evaluations should be monthly performed. Our Institution has a team of hematologists and other dedicated specialists that work together during the planning, conception, pregnancy, delivery and immediate post-delivery processes to assure best care to mother and child.
Conclusions
Survival of hemoglobinopathic patients in developed countries is improving and patients aspire to reproductive aims of their healthy peers.
TM and SCD patients often request fertility and pregnancy information, including screening of partners. We provide insights regarding reproductive health experience of hemoglobinopathies in both genders. Detailed results, mothers and child follow up and practical management will be presented.
Abruzzese:Incyte:Consultancy, Membership on an entity's Board of Directors or advisory committees;Pfizer:Consultancy, Membership on an entity's Board of Directors or advisory committees;Novartis:Consultancy, Membership on an entity's Board of Directors or advisory committees;Bms:Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal